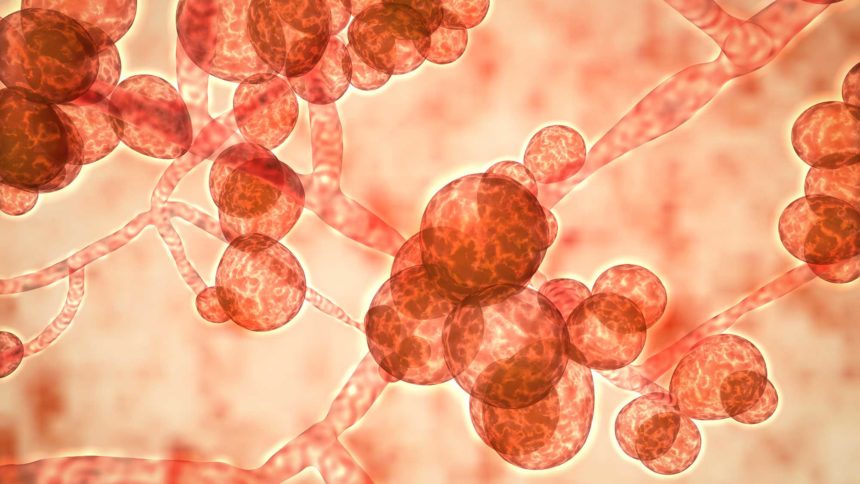
Patients who harbor the deadly candida auris fungus can shed it along with their skin and contaminate their surroundings, according to new research conducted in a Chicago skilled nursing facility.
Candida auris resists not only antifungal drugs, but also cleaning efforts, and has been found on surfaces all over affected facilities. Investigators have not been sure how the fungus spreads, but shedding skin may explain the extensive contamination that often occurs during outbreaks, said researchers from the Centers for Disease Control and Prevention who studied the problem in collaboration with Chicago’s Department of Health.
Twenty-eight people were tested at a ventilator-capable skilled nursing facility that was battling an outbreak. Beginning with a single case in March 2017, the illness had spread to 71% of its residents, despite disinfection attempts. Investigators were able to culture live fungus from the beds of all patients who tested positive and also from beds that were no longer occupied by patients who had tested positive.
“This finding supported our hypothesis that patients are actively shedding C. auris cells into their environment,” said study lead Joe Sexton, Ph.D., of the CDC’s Mycotic Diseases Branch.
Candida auris is highly contagious and tends to infect those who are the most vulnerable, including those with multiple medical conditions in hospitals and long-term skilled nursing facilities. It may be responsible for up to 60% of the deaths of those who become invasively infected, the CDC states. Highly susceptible patients include post-surgical patients, those with diabetes and those who have recently used antibiotics and antifungal medications. At greatest risk are patients with tubes and lines going into the body, according to the American Council on Science and Health.
“These results should be considered in developing more effective strategies for infection control efforts during a C. auris outbreak,” concluded Sexton.
Read the study abstract



